Alcohol-Based Sanitizer: What It Is, How It Works, and Why It Matters
When you reach for an alcohol-based sanitizer, a liquid or gel designed to kill germs on skin without water. Also known as hand sanitizer, it's one of the most common tools for stopping germs from spreading—especially in hospitals, schools, and public spaces. But not all of them work the same way. The real difference comes down to one number: alcohol concentration. If it’s below 60%, it won’t kill most viruses and bacteria. The CDC and WHO both say you need at least 60% ethanol or isopropanol to be effective. Anything less is just scented water with a fancy bottle.
Most alcohol-based sanitizer, a liquid or gel designed to kill germs on skin without water. Also known as hand sanitizer, it's one of the most common tools for stopping germs from spreading—especially in hospitals, schools, and public spaces. relies on alcohol to break open the outer shells of microbes. Ethanol and isopropanol are the two main types used. Ethanol works faster on some viruses, while isopropanol is better at killing bacteria. Both evaporate quickly, which means they don’t leave residue—but also means you need to rub your hands until they’re dry. If you stop before they’re dry, you didn’t kill enough germs. And no, wiping your hands on your shirt afterward doesn’t help. It just spreads what’s left.
Some products claim to be "antibacterial" or "kills 99.9% of germs," but those claims don’t mean much if the alcohol level is too low. The FDA cracked down on hundreds of hand sanitizers during the pandemic that contained methanol—poisonous stuff that can cause blindness or death if absorbed through the skin. Even if it smells fine, if you bought it from a random online seller or a gas station shelf with no brand name, it might be dangerous. Always check the FDA’s list of unsafe products before buying.
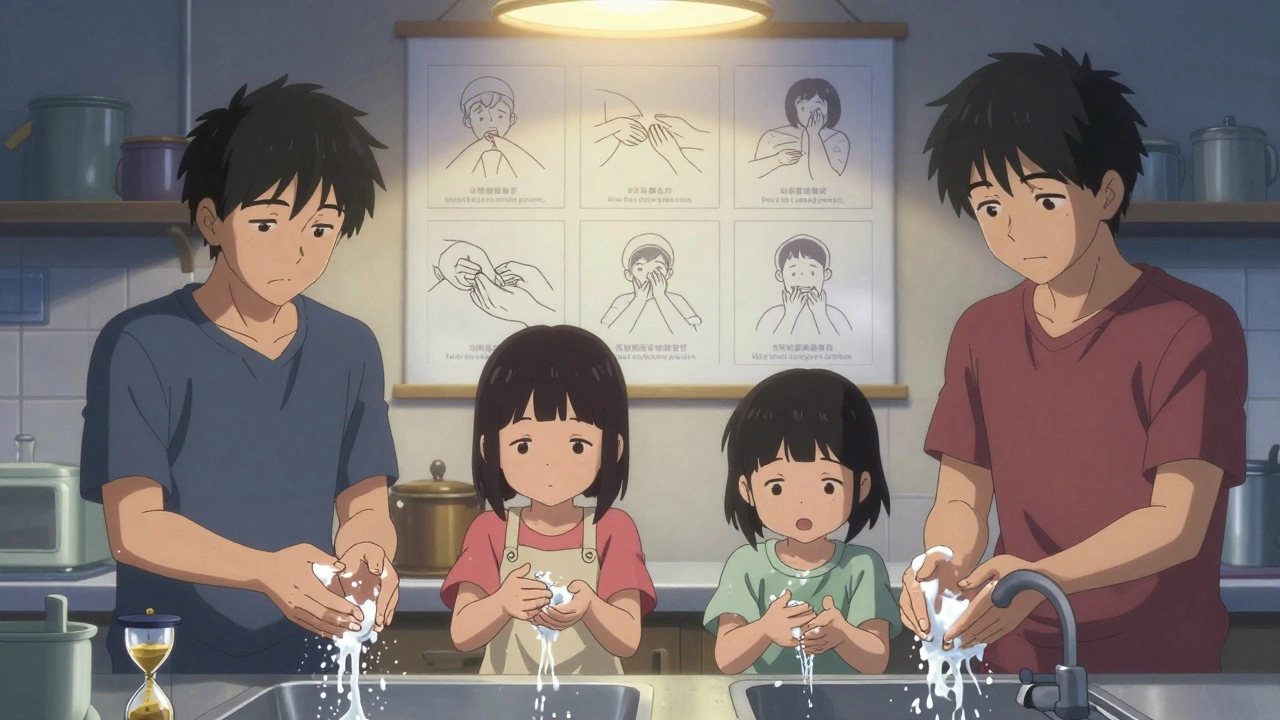
Alcohol-based sanitizer is great when you’re on the go, but it’s not a replacement for soap and water. If your hands are greasy, dirty, or covered in mucus, sanitizer won’t wash it away. Soap physically removes germs and debris. Sanitizer just kills what’s on the surface. That’s why health workers wash their hands before and after every patient—and use sanitizer in between. It’s a two-step system: clean first, then disinfect.
And here’s something most people don’t think about: frequent use can dry out your skin. That’s not just annoying—it’s risky. Cracked skin lets germs in. That’s why many hospital-grade sanitizers now include moisturizers like aloe or glycerin. You don’t need fancy ingredients, but if your hands feel tight or flaky after using it, you’re probably overdoing it. Try using less, or switch to one with added emollients.
There’s also the issue of storage. Alcohol evaporates over time, especially in heat. If you leave a bottle in your car on a summer day, the alcohol might boil off, leaving you with a useless product. Always check the expiration date, and store it in a cool, dark place. And never mix it with other cleaners—especially bleach. That creates chlorine gas, which can burn your lungs.
What you’ll find in the posts below are real, practical insights into how alcohol-based sanitizer fits into broader health practices—from safe disposal methods to how it compares to other disinfectants, and why some products fail even when they look right. You’ll learn what to look for on the label, which brands actually meet standards, and how to avoid being misled by marketing claims. This isn’t about fear—it’s about knowing what works, what doesn’t, and how to protect yourself without wasting money or risking your health.