When a life-saving medication disappears from the pharmacy shelf, patients don’t just feel frustrated-they feel abandoned. In 2023, nearly 300 drugs were in short supply across the U.S., with heart medications and cancer treatments among the most affected. But the real crisis isn’t just the lack of pills-it’s the silence that follows. Too often, patients walk into their doctor’s office or call their pharmacy only to be told, "We don’t have your medicine anymore." No explanation. No plan. No empathy. That’s not just poor service-it’s a breach of trust.
What Providers Are Legally and Ethically Required to Do
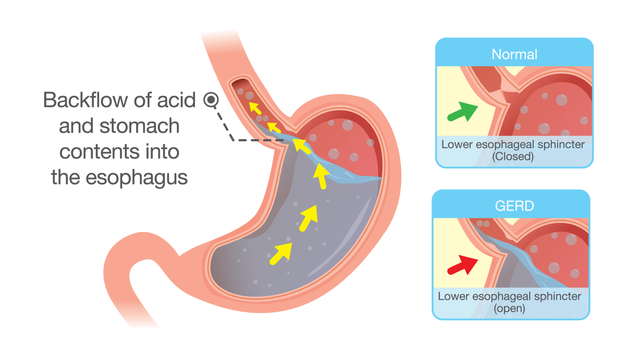
Healthcare providers aren’t just expected to handle drug shortages-they’re required to. The FDA’s 2012 Safety and Innovation Act forces manufacturers to report potential shortages months in advance. That gives providers time to prepare. But many don’t. The Joint Commission, which accredits U.S. hospitals, now lists structured communication during shortages as a National Patient Safety Goal. Starting in January 2025, facilities that fail to have clear protocols in place risk losing their accreditation. The European Medicines Agency set a clear standard in 2022: when a shortage hits, providers must tell patients exactly what’s missing, why, how long it might last, and what alternatives exist. This isn’t optional. It’s the baseline. And it’s not just about legal compliance-it’s about keeping people alive. A patient on a blood thinner who switches to an unfamiliar drug without understanding why is at risk of a stroke. A cancer patient given a substitute without knowing its side effects may stop treatment altogether.What Good Communication Looks Like
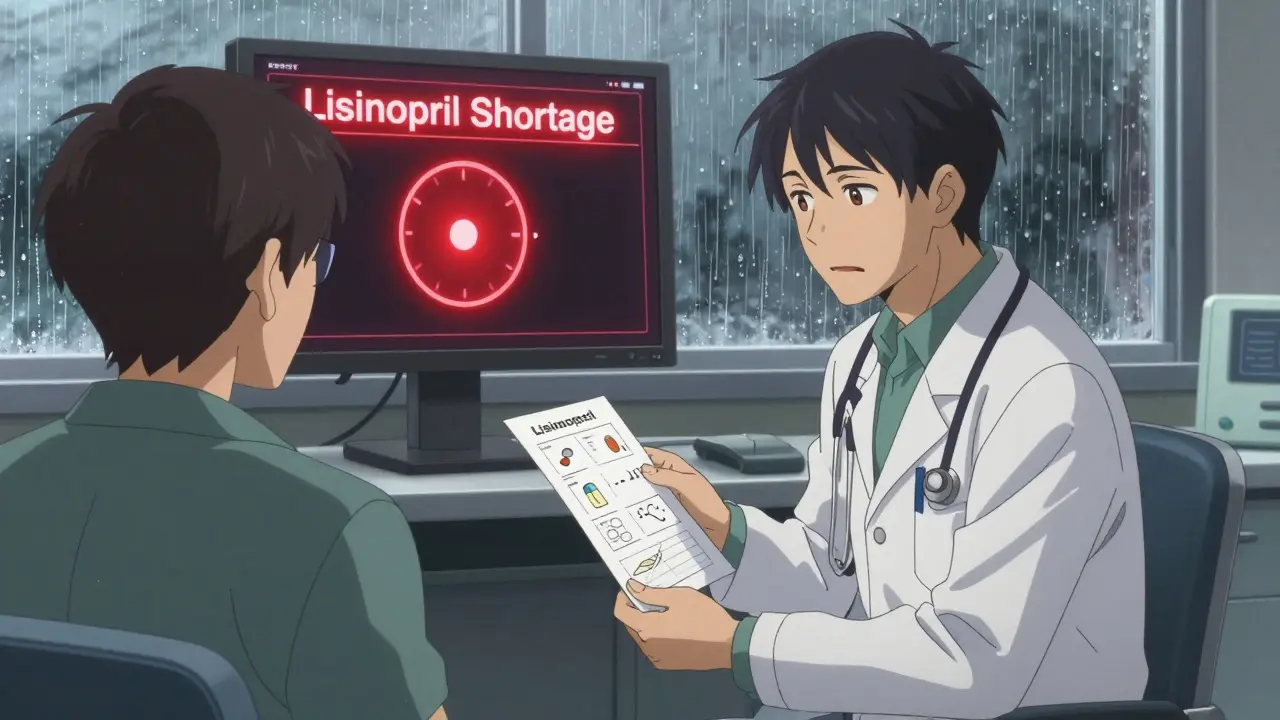
Good communication during a shortage isn’t a quick note on a prescription. It’s a conversation. The CDC recommends the "Chunk, Check, Change" method: break information into small pieces, confirm understanding, and adjust based on the patient’s reaction. For example:- Chunk: "Your usual heart medication, lisinopril, is currently unavailable nationwide."
- Check: "Can you tell me in your own words how this change might affect you?"
- Change: If the patient looks confused, switch to a visual aid-a simple chart comparing the old and new drug’s effects.
What Happens When Communication Fails
When providers stay silent, patients turn to Google. Or Reddit. Or their neighbors. And what they find isn’t reassuring. On Reddit’s r/healthcare, a post titled "When my heart medication disappeared" got over 1,200 upvotes and nearly 90 comments. Most patients described being handed a new pill with no context. "They just said, ‘Here, take this.’ I had no idea if it was safe," one wrote. On Healthgrades, reviews mentioning drug shortages average just 2.1 stars-far below the site’s overall 3.8-star average. The top complaints? "No warning before my refill was denied" and "The pharmacist seemed as confused as I was." The emotional toll is real. Patients report increased anxiety, fear of side effects, and loss of trust in their providers. Dr. Jane Smith from Johns Hopkins says 73% of patients feel less confident in their care when shortages aren’t explained upfront. That’s not just bad for morale-it’s bad for health. Studies show patients who understand their alternatives are 83% more likely to stick with their treatment plan. Those who don’t? They stop taking their meds.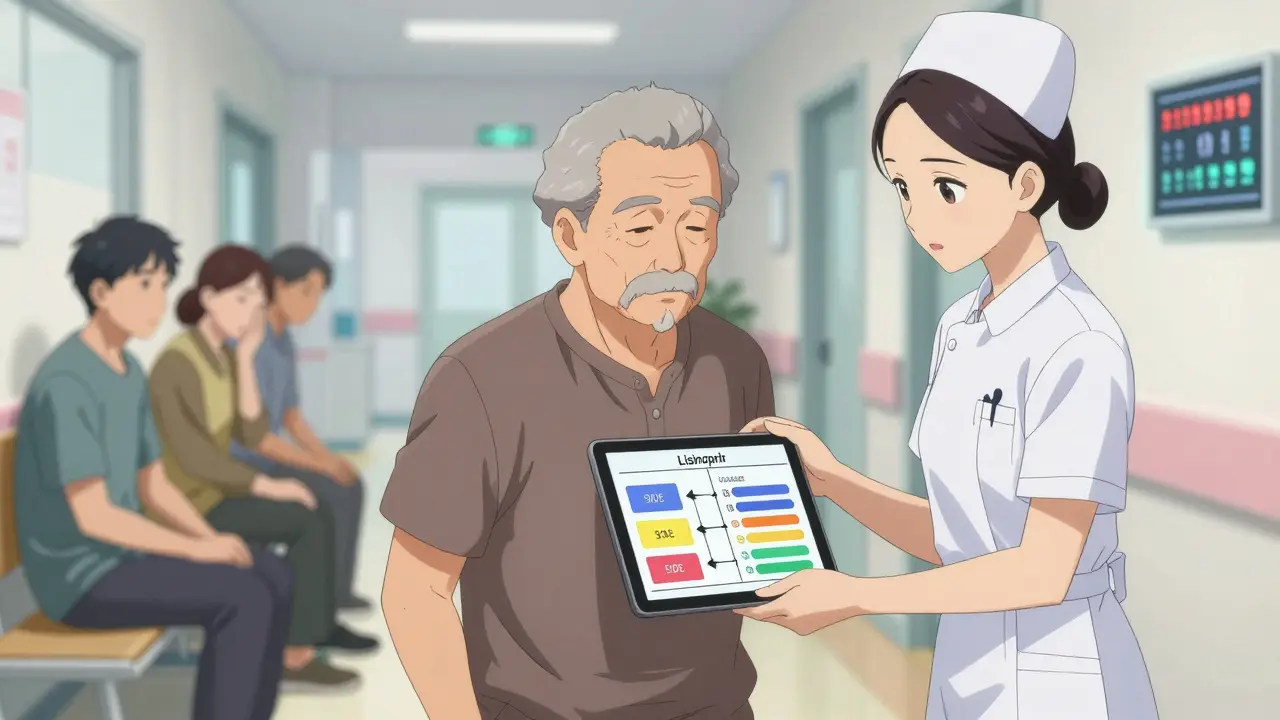
Barriers That Make Communication Hard
It’s not that providers don’t care. Many are overwhelmed. The average doctor visit lasts just 15.7 minutes. Fitting in a detailed shortage discussion? Nearly impossible without support. Electronic health records (EHRs) make it worse. Only 38% of systems can flag when a drug is in short supply. That means providers often find out about shortages at the same time as patients-right before the appointment. Rural clinics face even bigger hurdles: 68% of providers there say they have no real-time access to shortage updates. Language and literacy are major barriers too. Nearly half of U.S. adults struggle with health information. If a patient reads at a 4th-grade level, a 10-page pamphlet on drug alternatives is useless. The CDC says all shortage materials must be written at a 6th- to 8th-grade level. No jargon. No Latin names. Just clear, simple language.What Works: Real Solutions from Real Clinics
Some places are getting it right. Mayo Clinic uses a system called SHIP-Shortage Handling and Information Protocol. Every time a drug shortage is confirmed, the system automatically generates a patient letter, a provider talking point, and a pharmacy alert. Nurses review each case. Patients get a follow-up call. Result? 87% satisfaction. Kaiser Permanente built shortage notifications into routine visits. Instead of adding time, they integrated the conversation into existing workflows. Now, it takes just 2.7 extra minutes per patient. Intermountain Healthcare created an EHR template that auto-fills shortage details: drug name, reason, alternative, expected return date. No typing. No forgetting. Just one click. At Memorial Sloan Kettering, communication specialists handle all cancer drug shortages. They’re trained in empathy, grief, and complex medical info. They don’t just explain options-they listen. And they follow up.
What Patients Really Want
A 2022 survey of 2,400 patients found three things matter most when a medication disappears:- Clear reason why (78% say this is critical)
- Proof the alternative works (72%)
- When the original might come back (65%)
The Future Is Here
The market for shortage communication tools is growing fast-from $147 million in 2022 to over $300 million by 2027. Why? Because payers like Medicare are starting to tie reimbursement to how well providers handle shortages. Poor communication? Lower payments. Good communication? Better scores, more funding. AI is starting to help too. Fifteen major health systems are testing tools that predict shortages before they happen, using supply chain data, manufacturing reports, and even weather patterns that affect drug production. And by late 2024, the International Pharmaceutical Federation plans to release standardized patient communication templates-free, easy to use, and available in multiple languages. That’s a game-changer for small clinics and rural hospitals.What You Can Do Today
If you’re a provider:- Ask your EHR vendor: Can it flag drug shortages?
- Start using plain language. No "angiotensin-converting enzyme inhibitors." Say "blood pressure pill."
- Use the teach-back method: "Can you explain how you’ll take this new pill?"
- Keep a one-page handout ready for common shortages-lisinopril, metformin, levothyroxine.
- Ask your pharmacist: "Is this drug in short supply?"
- Ask your doctor: "Why are we switching? Is this as safe as my old one? When will the original be back?"
- Write down your questions. Don’t be afraid to ask them twice.
What should I do if my medication is suddenly unavailable?
Don’t stop taking your medicine without talking to your provider. Call your doctor’s office or pharmacist right away. Ask: Why is it unavailable? What’s the alternative? Is it safe? Will it work the same way? And when might the original come back? Write down the answers. If you’re unsure, ask for a printed handout or email summary.
Are generic drugs just as good as brand names during a shortage?
Yes, when they’re approved by the FDA. Generic drugs must meet the same standards as brand names for safety, strength, and effectiveness. The only differences are in inactive ingredients like fillers or dyes-which rarely affect how the drug works. But if you’ve had a reaction to a specific generic before, tell your provider. Not all generics are made the same way.
Why don’t pharmacies just tell me about shortages ahead of time?
Many pharmacies don’t have real-time access to shortage data. Manufacturers report shortages to the FDA, but that information doesn’t always reach pharmacies until it’s too late. Some pharmacies use third-party tools, but not all do. The best way to stay informed is to ask your provider to notify you in advance if a drug you take is at risk.
Can I get my original medication from another country if it’s unavailable here?
Importing medications from other countries is illegal in the U.S. unless under very limited exceptions. Even if you find a website selling your drug cheaper, it may be fake, expired, or contaminated. The FDA warns against buying medications online from overseas pharmacies. Talk to your provider about FDA-approved alternatives instead.
How do I know if my new medication is working the same way?
Ask your provider what signs to watch for. For example, if you’re switching from one blood pressure drug to another, your provider might ask you to check your blood pressure at home weekly for the first month. They may also order a blood test or adjust your dose. Don’t assume it’s working just because you’re taking it. Follow up as advised.
Is there a government database I can check for drug shortages?
Yes. The FDA maintains a public Drug Shortages page that lists current and resolved shortages. You can search by drug name, manufacturer, or category. But remember: the list doesn’t always reflect what’s available at your local pharmacy. Use it as a reference, not a guarantee. Always confirm with your provider or pharmacist.