
Non-Opioid Treatment Effectiveness Calculator
Find Your Best Non-Opioid Treatment
Select your pain type and severity to see which non-opioid options are most effective for you based on current research.
Recommended Treatment Options
How this works: Based on CDC guidelines and recent research, we've identified treatments that provide the best balance of effectiveness and safety for your specific pain type.
What to Expect
For millions of people living with chronic pain, opioids are no longer the go-to solution. The risks - addiction, overdose, tolerance, and side effects like constipation and drowsiness - are too high. And the truth? Opioids often don’t work well for long-term pain like arthritis, back pain, or nerve pain. The non-opioid pain management options available today aren’t just safer - in many cases, they work just as well, if not better.
What Works Better Than Opioids for Chronic Pain?
Research from the CDC’s 2022 guidelines is clear: non-opioid treatments should come first. A 2022 study in JAMA Network Open followed over 200 people with chronic back or joint pain for a year. Those on non-opioid treatments reported the same level of pain relief and improved function as those on opioids - but with nearly 40% fewer side effects. That’s not a small difference. It’s life-changing.
Here’s what actually works:
- Exercise therapy - Whether it’s walking, swimming, or strength training, moving your body reduces pain signals over time. Physical therapists design programs that start gentle and build up. Most people see results after 6-8 weeks of 2-3 sessions per week.
- Cognitive behavioral therapy (CBT) - This isn’t just "thinking positive." CBT teaches you how pain affects your brain and how to break the cycle of fear and avoidance. Eight to twelve weekly sessions can cut pain intensity by 30-50% for many.
- Acupuncture - Used for thousands of years, it’s now backed by solid science. Studies show it helps with osteoarthritis, migraines, and lower back pain. Many patients report fewer pain flare-ups after a series of 8-10 treatments.
- Yoga and tai chi - These mind-body practices improve flexibility, balance, and reduce stress hormones that make pain feel worse. People with fibromyalgia often find these the most sustainable options.
- Massage and spinal manipulation - Especially helpful for muscle tension and neck or lower back pain. Regular sessions (once a week for 4-6 weeks) can reduce reliance on painkillers.
Non-Opioid Medications That Actually Help
Not everyone wants to rely only on movement and therapy. That’s where non-opioid medications come in - and they’re not just aspirin and Tylenol anymore.
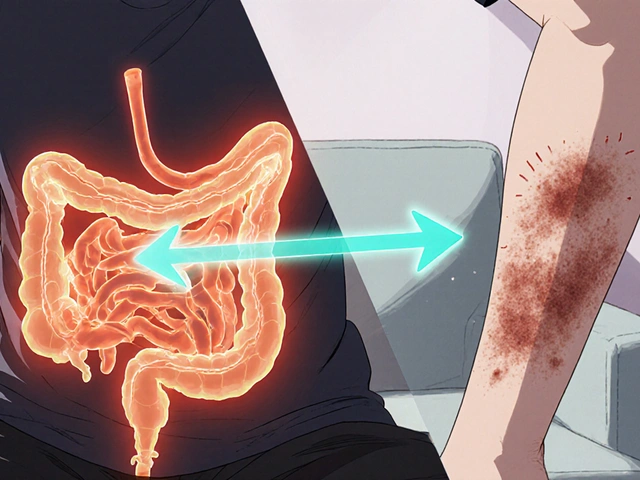
- NSAIDs (ibuprofen, naproxen) - Great for inflammation-related pain like arthritis. But don’t take them long-term without checking with your doctor. They can irritate your stomach or affect your kidneys, especially if you’re over 65.
- Acetaminophen (Tylenol) - Safer for your stomach than NSAIDs, but too much can damage your liver. Stick to 3,000-4,000 mg per day max, and avoid alcohol.
- Duloxetine (Cymbalta) and venlafaxine (Effexor) - Originally antidepressants, these SNRIs are now first-line for nerve pain and chronic musculoskeletal pain. They don’t make you "happy" - they change how your nerves send pain signals. It takes 4-6 weeks to kick in, but many report 30-50% pain reduction.
- Pregabalin (Lyrica) and gabapentin - These are go-to drugs for nerve pain from diabetes, shingles, or sciatica. About 30-50% of users get meaningful relief. Side effects? Drowsiness and weight gain are common - so start low and go slow.
- Topical treatments - Capsaicin cream (from chili peppers) and lidocaine patches deliver pain relief right where you need it, with almost no system-wide side effects. Great for localized pain like knee arthritis or post-shingles pain.
In October 2023, the FDA approved a new drug called suzetrigine (brand name Journavx). It’s the first novel non-opioid painkiller in over 20 years, designed specifically for moderate to severe acute pain - like after surgery or a broken bone. It works by blocking sodium channels in nerves, not by affecting the brain like opioids do. This is a big deal.
What’s Holding People Back?
Even though these options work, many people still can’t access them. Why?
- Insurance won’t cover it - Medicare covers 80% of physical therapy after you hit your deductible, but private insurers often cap you at 15-20 visits a year. Acupuncture? Many require pre-approval. A 2022 U.S. Pain Foundation survey found 42% of patients gave up on non-opioid treatments because their insurance wouldn’t pay.
- It takes time - Unlike an opioid pill that works in 30 minutes, physical therapy, CBT, or even antidepressants need weeks to show results. People get discouraged and quit too soon.
- Not enough providers - In rural areas, there might not be a physical therapist within 50 miles. Psychologists who specialize in pain? Even scarcer. A 2023 study found 58% of rural U.S. counties lack access to physical therapists.
- Side effects from meds - Yes, non-opioid drugs have side effects too. NSAIDs can cause stomach bleeding. Pregabalin makes you sleepy. Duloxetine can cause nausea. But these are often manageable with dose adjustments - unlike opioid addiction, which can be deadly.

Real People, Real Results
On Reddit’s r/ChronicPain community, one user shared how they managed fibromyalgia without opioids: aquatic therapy three times a week, CBT, and low-dose naltrexone (an off-label use that helps regulate immune response). After 18 months, they went from being housebound to hiking again.
A Mayo Clinic Connect survey of 247 chronic pain patients found 68% got moderate to significant relief from physical therapy. Over half said acupuncture helped. But the same group also reported that 45% of NSAID users had stomach issues, and 62% of pregabalin users felt too drowsy to drive.
The message? There’s no magic bullet - but there are combinations that work. The key is personalization.
How to Start Your Non-Opioid Pain Plan
If you’re tired of opioids or worried about starting them, here’s how to begin:
- Talk to your doctor - Ask: "What non-opioid options do you recommend for my type of pain?" Bring up the CDC guidelines. Most providers now know them.
- Try one non-pharmacological option - Pick one: physical therapy, yoga, or CBT. Commit to 6-8 weeks. Don’t quit after two sessions.
- Consider one non-opioid medication - If pain is moderate to severe, ask about duloxetine or a topical patch. Don’t assume NSAIDs are enough.
- Track your progress - Use a simple journal: rate pain 1-10 daily, note what you did, and how you felt. Patterns emerge over time.
- Ask about support - The U.S. Pain Foundation and American Chronic Pain Association offer free resources and peer support groups. You’re not alone.

The Future Is Here - And It’s Non-Opioid
The global market for non-opioid pain treatments is growing fast - projected to hit $58 billion by 2030. Why? Because science, patients, and regulators are all on the same page.
The NIH has invested over $1.3 billion into developing new non-addictive pain drugs. More than 47 are in clinical trials right now. Experts predict we’ll soon have blood tests or brain scans to match patients with the right treatment - no trial and error.
And the policy shift is real. States like Florida now require doctors to tell patients about non-opioid options before prescribing opioids. The CDC’s message is loud and clear: non-opioid therapies aren’t just alternatives. They’re the standard of care.
For chronic pain, the old model - reach for the pill - is over. The new model is smarter, safer, and more sustainable. It takes effort. It takes time. But for many, it’s the only way to get back to living - without the risk of addiction or overdose.
Are non-opioid pain treatments really as effective as opioids?
Yes - for most chronic pain conditions like arthritis, back pain, and nerve pain. A 2022 study in JAMA Network Open found patients on non-opioid treatments reported the same level of pain relief and improved function as those on opioids - but with far fewer side effects. Opioids don’t work well long-term for chronic pain, and the risks often outweigh the benefits.
What’s the safest non-opioid painkiller?
There’s no single "safest" option - it depends on your health. Topical treatments like lidocaine patches or capsaicin cream have the least systemic risk. Acetaminophen is safer for your stomach than NSAIDs, but you must stay under 4,000 mg per day to protect your liver. For long-term use, non-pharmacological methods like exercise and CBT carry no medication risks at all.
How long does it take for non-opioid treatments to work?
It varies. Physical therapy and exercise usually show results in 6-8 weeks. Cognitive behavioral therapy takes 8-12 weekly sessions. Antidepressants like duloxetine can take 4-6 weeks to reduce pain signals. Topical creams and NSAIDs work faster - sometimes in hours or days - but aren’t ideal for long-term use. Patience is key.
Can I use non-opioid treatments if I’ve been on opioids before?
Absolutely. Many people successfully switch from opioids to non-opioid options. It often requires a gradual taper under medical supervision to avoid withdrawal. Combining therapies - like physical therapy with a low-dose SNRI - can help manage pain during the transition. Talk to a pain specialist to create a safe plan.
Why aren’t non-opioid treatments covered better by insurance?
Historically, insurance favored pills because they’re cheaper and easier to prescribe. Physical therapy, acupuncture, and psychological services cost more upfront and require multiple visits. But that’s changing. The CDC guidelines and state laws are pushing insurers to cover these options. Still, many plans limit visits or require prior authorization - so always check your benefits before starting.
Is there a new non-opioid pain drug I should know about?
Yes - suzetrigine (brand name Journavx), approved by the FDA in October 2023. It’s the first new non-opioid painkiller in over 20 years, designed for moderate to severe acute pain like after surgery. It works differently than opioids - targeting nerve signals without affecting the brain’s reward system. It’s not for long-term chronic pain yet, but it’s a major step forward.
What to Do Next
If you’re managing pain and want to avoid opioids, start small. Pick one non-opioid approach - maybe a weekly yoga class or a talk with your doctor about duloxetine. Track how you feel. Don’t expect overnight results. But if you stick with it, you might find something that doesn’t just numb your pain - it helps you live with it better.




Conor Forde
December 2, 2025 AT 07:35Okay but have y’all seen the price of a single physical therapy session? Like, I get it, ‘move more’ is the new mantra, but my insurance covers 3 visits a YEAR. So I’m supposed to just… stretch my way out of nerve pain? Cool. I’ll just hop on my yoga mat and manifest a pain-free spine while my landlord raises the rent. 😌
patrick sui
December 2, 2025 AT 16:58Interesting breakdown, but let’s not romanticize non-opioid modalities. CBT is great in theory, but when you’re in 8/10 pain daily, ‘reframing your thoughts’ feels like emotional gaslighting. And suzetrigine? Promising, but phase 3 trials are still small. We need real-world data, not hype. Also-why is everyone ignoring transcranial magnetic stimulation? It’s FDA-cleared, non-invasive, and works for 60% of neuropathic cases. Just saying.
Declan O Reilly
December 4, 2025 AT 15:59Man, I used to think pain was just something you endured. Then I tried tai chi after a bad car crash. At first, I thought it was nonsense-slow movements, breathing, all that zen crap. But after 10 weeks? My back stopped screaming. Not cured. Not gone. But quieter. Like a neighbor who stopped blasting EDM at 3am. It’s not magic. It’s just… different. And honestly? More human. We treat pain like a bug to exterminate. Maybe we should treat it like a misunderstood roommate.
Matt Dean
December 4, 2025 AT 16:38Wow. Just… wow. You people are still clinging to this hippie nonsense like it’s 2012. Exercise? Yoga? Acupuncture? Please. If your pain is bad enough to need meds, you don’t get to play ‘alternative lifestyle’-you need real medicine. And guess what? Opioids are still the most effective tool we have for severe pain. The CDC guidelines are politically motivated, not scientifically rigorous. Stop pretending you’re healing yourself with crystals and stretchy pants.
Walker Alvey
December 5, 2025 AT 14:32Oh look, another article telling me to ‘move more’ while my spine is literally collapsing. Congrats. You’ve written a 2000-word pamphlet for people who can’t afford physical therapy, can’t find a therapist who takes insurance, and don’t have the energy to walk to the mailbox. Meanwhile, the FDA approved a new drug that works but costs $12,000 a year. So yeah. Non-opioid options. Great. Just like free healthcare. In a dream.
Adrian Barnes
December 6, 2025 AT 02:36The fundamental flaw in this narrative is the assumption that efficacy is the only metric that matters. It is not. The societal cost of chronic pain is not measured in pain scores alone-it is measured in lost productivity, ER visits, disability claims, and opioid dependency cascades. Non-opioid interventions, while marginally effective for some, lack scalability, standardization, and reproducibility across heterogeneous populations. The data cherry-picked here ignores the 40% of patients who derive zero benefit from CBT or acupuncture. This is not medicine. It is wishful thinking dressed in wellness branding.
James Steele
December 7, 2025 AT 22:21Let’s be real-the entire non-opioid movement is a corporate rebranding play. Big Pharma can’t sell opioids anymore? Fine. Let’s sell $800/month SNRIs, $150/visit acupuncture, and $2000/year yoga memberships. Meanwhile, the real solution-better pain neuroscience education for clinicians-isn’t even on the table. Suzetrigine? Cute. But it’s just another molecule in a long line of ‘revolutionary’ drugs that get pulled after Phase 4 because they cause arrhythmias. We’re not solving the problem. We’re just repackaging it.
Shannon Gabrielle
December 8, 2025 AT 20:06Y’all are so naive. You think insurance won’t cover PT because it’s expensive? Nah. It’s because they don’t want you to get better. If you’re pain-free, you go back to work. If you go back to work, you stop collecting disability. And if you stop collecting disability? That’s $12,000 per person per year the system doesn’t have to pay. So they make you wait 6 months for a referral, then cap you at 10 visits. It’s not about health. It’s about money. And you’re just the patsy.
ANN JACOBS
December 10, 2025 AT 04:39Thank you for this comprehensive and deeply researched overview. I have personally benefited from duloxetine and weekly aquatic therapy after a spinal fusion, and I can attest that the journey is slow, often frustrating, and requires immense patience-but the outcome is sustainable. Unlike opioids, which created a dependency that felt like a slow surrender of my autonomy, these modalities restored my sense of agency. I now track my pain daily using a simple app, and I’ve noticed patterns: stress spikes correlate with flare-ups, and even 15 minutes of stretching before bed reduces nighttime awakenings. I encourage anyone reading this to view this not as a treatment plan, but as a reclamation of your life-one small, consistent action at a time. You are not broken. You are adapting.
Nnaemeka Kingsley
December 11, 2025 AT 20:12Bro in Nigeria we don’t even have PT clinics. My uncle has back pain since 2018. He use ginger tea and hot water bottle. Now he walk again. No doctor. No pill. Just family care. Maybe the real solution is not more drugs or fancy therapy but community. We forget that.
Kshitij Shah
December 12, 2025 AT 17:56Man, in India we’ve had ayurveda and yoga for 5000 years and now you’re treating it like a new trend? Also, why is everyone ignoring the fact that most chronic pain comes from sitting in chairs all day? No amount of acupuncture fixes a 12-hour desk posture. Go stand up. Walk. Stop blaming the pain. Blame the capitalism that made you a desk zombie.
Sean McCarthy
December 12, 2025 AT 19:17Acupuncture? Really? It’s a placebo. The needles don’t even go into the right meridians. And CBT? That’s just telling people to ‘think differently’ while their body is literally screaming. This article is a waste of time. If you’re in real pain, you need real medication. Not yoga. Not ‘mindfulness.’ Not a ‘journey.’ Just a damn pill that works.
Jaswinder Singh
December 12, 2025 AT 22:03U all talkin’ like pain is some abstract concept. I’ve been on 3 opioids in 5 years. Lost my job. My wife left. My kid don’t know me. I tried CBT. Felt like talking to a robot. PT? I couldn’t even get outta bed. Then I found a guy in Punjab who does pressure point massage with mustard oil. 3 weeks. I cried. Not from pain. From feeling my leg again. You don’t need FDA approval to heal. You need someone who sees you.
Bee Floyd
December 13, 2025 AT 04:33I appreciate the nuance here. I’m not a fan of the ‘either/or’ framing-opioids bad, alternatives good. It’s messy. Some people need opioids short-term. Some need acupuncture for life. The real issue? We don’t have integrated pain clinics. We have specialists who treat one piece. Pain isn’t just a nerve. It’s sleep, stress, trauma, isolation. We need teams-doctors, therapists, social workers, peer mentors-all in one room. Until then, we’re just rearranging deck chairs on the Titanic.
Jeremy Butler
December 15, 2025 AT 00:56The assertion that non-opioid interventions are ‘equally effective’ is statistically misleading. The JAMA study referenced employed a non-inferiority design with a margin of 1.5 points on the VAS scale-a threshold that lacks clinical significance. Furthermore, the attrition rate in the non-opioid arm was 37%, suggesting that the cohort was not representative of the broader chronic pain population. The FDA’s approval of suzetrigine, while commendable, was based on a Phase 2 trial with n=182. Until large-scale, longitudinal, real-world evidence is available, we are engaging in therapeutic optimism, not evidence-based medicine.