Understanding Emphysema and Its Impact on Pregnancy
As a mother-to-be, it's important to be aware of the potential health risks that could affect you and your unborn baby. One such health concern is emphysema, a chronic lung disease that can have a significant impact on pregnancy. In this section, we'll explore what emphysema is, how it affects the body, and the potential complications it can cause during pregnancy.
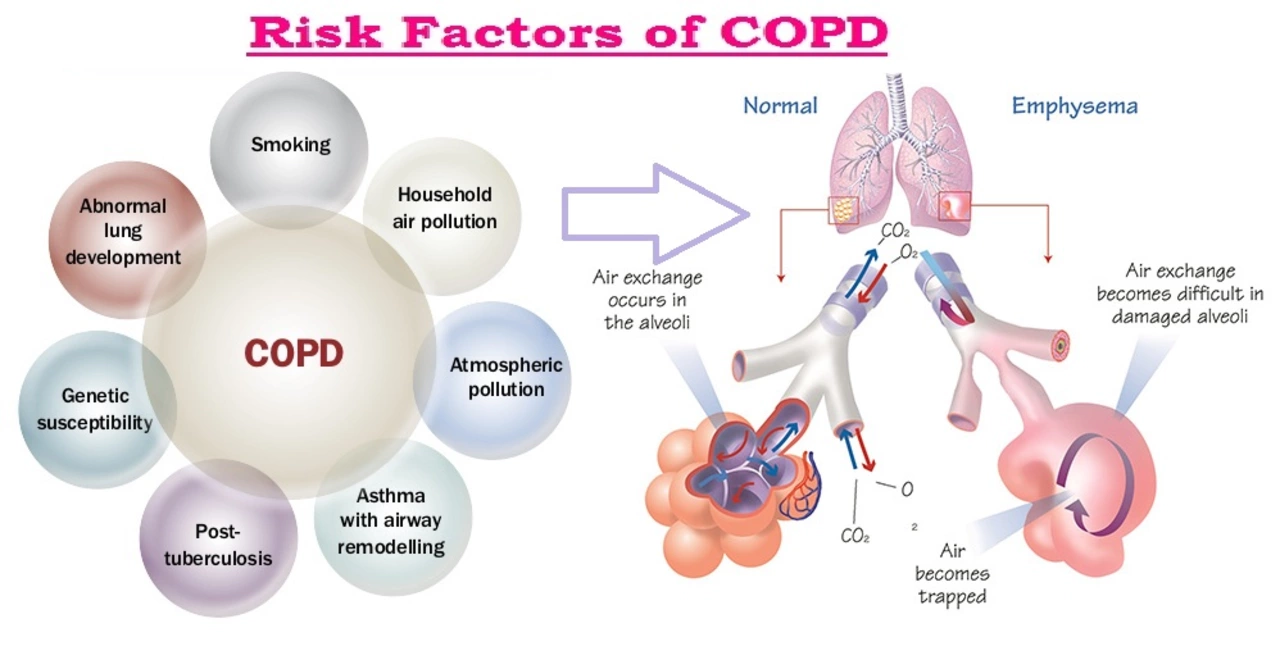
Emphysema is a type of chronic obstructive pulmonary disease (COPD) characterized by damage to the air sacs (alveoli) in the lungs. This damage leads to difficulty in breathing and a decreased ability to exchange oxygen and carbon dioxide in the lungs. People with emphysema often experience shortness of breath, coughing, and wheezing. The primary cause of emphysema is long-term exposure to irritants such as cigarette smoke, air pollution, and certain occupational chemicals.
Pregnant women with emphysema may face several challenges, including a higher risk of premature birth, low birth weight, and other complications. The decreased oxygen levels in the mother's blood can also affect the baby's growth and development, possibly leading to long-term health issues.
Managing Emphysema During Pregnancy
Proper management of emphysema during pregnancy is crucial to ensure the health and well-being of both the mother and the baby. By working closely with your healthcare team, you can develop a comprehensive plan to manage your condition effectively throughout your pregnancy. In this section, we'll discuss some of the key strategies to help you manage emphysema while you're expecting.
First and foremost, it's essential to quit smoking if you haven't already. Smoking is the leading cause of emphysema, and continuing to smoke during pregnancy can exacerbate the condition and increase the risk of complications. Your healthcare provider can provide resources and support to help you quit for good.
Another important aspect of managing emphysema during pregnancy is maintaining regular prenatal check-ups with your healthcare provider. They will closely monitor your lung function and overall health, adjusting your treatment plan as necessary. This may include the use of medications, oxygen therapy, or pulmonary rehabilitation to help you breathe more easily.
Additionally, maintaining a healthy lifestyle is essential for pregnant women with emphysema. Eating a balanced diet, staying physically active, and getting enough rest can help improve your overall health and reduce the risk of complications.
Preparing for Delivery with Emphysema
As your due date approaches, it's important to be prepared for the delivery process, especially if you have emphysema. In this section, we'll discuss some of the steps you can take to ensure a smooth and safe delivery for both you and your baby.
One of the first things to consider is choosing a healthcare team experienced in managing high-risk pregnancies and emphysema. This may include an obstetrician, pulmonologist, and neonatologist who can work together to create a personalized delivery plan tailored to your needs and the needs of your baby.
It's also essential to discuss pain management options with your healthcare team, as certain medications may affect your breathing during labor and delivery. Together, you can create a plan that balances effective pain relief with minimal impact on your lung function.
Finally, be prepared for the possibility of a cesarean section delivery if your healthcare team determines it is the safest option for you and your baby. This decision will be based on your individual circumstances, including the severity of your emphysema and any potential complications that may arise during labor.
Postpartum Care for Mothers with Emphysema
After your baby is born, it's essential to continue managing your emphysema and to receive appropriate postpartum care. In this section, we'll discuss some important aspects of postpartum care for mothers with emphysema to help you maintain your health and well-being during this critical time.
First, continue to work closely with your healthcare team to monitor your lung function and overall health. They may adjust your treatment plan as needed, including changes in medication or oxygen therapy. Be sure to attend all scheduled postpartum check-ups and follow your healthcare provider's recommendations carefully.
It's also important to prioritize self-care during the postpartum period. This includes eating a balanced diet, staying active, and getting enough rest. Taking care of yourself will help you recover from childbirth and manage your emphysema more effectively.
If you're breastfeeding, discuss any medications you're taking for emphysema with your healthcare provider to ensure they are safe for your baby. They may recommend adjustments to your treatment plan to minimize any potential risks to your baby.
Support and Resources for Pregnant Women with Emphysema
Living with emphysema while pregnant can be challenging, but you don't have to face it alone. There are many resources and support networks available to help you navigate this journey. In this section, we'll discuss some of the best sources of support and information for pregnant women with emphysema.
Your healthcare team is an invaluable resource for information and guidance throughout your pregnancy. Don't hesitate to ask questions and express any concerns you may have. They can provide personalized advice and help you find additional resources if needed.
Online forums and support groups can also be helpful in connecting with other pregnant women who have emphysema or other lung conditions. These communities can offer practical advice, encouragement, and understanding from people who have faced similar challenges.
Finally, national and local organizations, such as the American Lung Association and the COPD Foundation, can provide educational materials, support programs, and advocacy opportunities for people living with lung diseases like emphysema. By educating yourself and connecting with others, you can be better prepared to face the challenges of emphysema and pregnancy.




Ria Ayu
May 21, 2023 AT 09:03Reading through this guide reminded me how fragile the balance between maternal health and fetal development truly is. Emphysema adds another layer of complexity that deserves thoughtful attention. I appreciate the calm tone and the practical steps suggested for prenatal care. Remember to breathe deeply, both literally and metaphorically, as you navigate this journey.
maya steele
May 24, 2023 AT 05:07This article does a commendable job outlining the clinical considerations for pregnant patients with emphysema. It highlights the importance of smoking cessation, which remains the cornerstone of management. The discussion on oxygen therapy and pulmonary rehabilitation is thorough and evidence‑based. Regular monitoring of lung function, as suggested, can preempt many complications. Moreover, the emphasis on a multidisciplinary team aligns with best practice guidelines. The section on delivery planning thoughtfully addresses analgesia options and the potential need for cesarean delivery. Postpartum follow‑up recommendations are also well articulated. Overall, this serves as a solid reference for both patients and clinicians.
Sharon Lax
May 27, 2023 AT 01:10Obstructive lung pathology during gestation intensifies peri‑natal risk matrices.
paulette pyla
May 29, 2023 AT 21:13Ah yes, because every obstetrician has a spare pulmonary specialist on speed‑dial, right? The article’s “multidisciplinary team” sounds more like a wish list than a realistic scenario for most patients. But sure, let’s assume everyone can afford top‑tier oxygen tanks and personalized rehab sessions. 🙄
Benjamin Cook
June 1, 2023 AT 17:17Wow!!! This is sooo helpful!!! I love how it breaks down each stage!!! Can't wait to share with my sister!!!
karthik rao
June 4, 2023 AT 13:20While enthusiasm is commendable, it is essential to convey information accurately. Over‑excitement may obscure nuanced medical advice. Please ensure that dosage and therapy details are double‑checked. 😊👍
Breanne McNitt
June 7, 2023 AT 09:23I found the sections on lifestyle adjustments particularly useful. Balancing nutrition, mild exercise, and stress reduction can make a big difference. It’s also encouraging to see the mention of support groups, which can provide emotional solidarity. Thanks for the well‑rounded perspective.
Ashika Amirta varsha Balasubramanian
June 10, 2023 AT 05:27Your point about community support resonates deeply. In many South Asian families, collective caregiving is a strength we can harness. Encouraging relatives to participate in prenatal visits can also improve adherence to treatment plans.
Jacqueline von Zwehl
June 13, 2023 AT 01:30The article’s structure is clear, and the language is accessible. I especially appreciate the brief explanation of alveolar damage. It helps non‑medical readers grasp the core issue without feeling overwhelmed.
Christopher Ellis
June 15, 2023 AT 21:33Sure but it glosses over the pharmacologic complexities of COPD in pregnancy.
kathy v
June 18, 2023 AT 17:37The topic of emphysema in pregnancy is seldom given the attention it warrants in mainstream medical discourse. This oversight is especially troubling given the rising prevalence of chronic lung disease among women of childbearing age. When a pregnant patient presents with compromised pulmonary function, the stakes rise dramatically for both mother and fetus. Oxygen deprivation can precipitate pre‑eclampsia, intrauterine growth restriction, and even stillbirth if not meticulously managed. Moreover, the physiological changes of pregnancy-namely increased blood volume and diaphragmatic elevation-exacerbate the already limited respiratory reserve of an emphysema patient. From a public health perspective, smoking cessation programs must be integrated into prenatal care pathways rather than treated as peripheral counseling. The multidisciplinary model advocated in the article is a step in the right direction, but it requires systemic support to be truly effective. Rural hospitals, for instance, often lack on‑site pulmonologists, forcing patients to travel great distances for specialized care. Telemedicine offers a promising bridge, enabling remote monitoring of spirometry and oxygen saturation in real time. Insurance coverage, however, remains a significant barrier, with many plans refusing to reimburse home oxygen equipment for pregnant patients. Legislative advocacy is therefore essential to mandate equitable access to life‑saving therapies. From an ethical standpoint, clinicians must balance maternal autonomy with fetal beneficence, a dilemma that is rarely black and white. Informed consent discussions should explicitly cover the potential need for early delivery if maternal respiratory decompensation occurs. The psychosocial impact cannot be understated; anxiety and isolation often accompany chronic illness during pregnancy. Ultimately, a comprehensive approach that blends medical, social, and policy interventions will yield the best outcomes for both mother and child.
Jorge Hernandez
June 21, 2023 AT 13:40Totally agree 🙌! Telehealth could really change the game for these moms.
Raina Purnama
June 24, 2023 AT 09:43I think the piece could include more resources for low‑income patients, such as community health center programs.
April Yslava
June 27, 2023 AT 05:47It’s no coincidence that big pharma pushes expensive inhalers while ignoring affordable community clinics. The system is rigged to profit from our suffering, and we must demand transparency.
Daryl Foran
June 30, 2023 AT 01:50These so‑called “best practices” are a collection of buzzwords that lack real‑world applicability. Most clinicians will never implement such exhaustive protocols.
Rebecca Bissett
July 2, 2023 AT 21:53Great read!!!
Michael Dion
July 5, 2023 AT 17:57It could be better
Trina Smith
July 8, 2023 AT 14:00I appreciate the thoroughness of this guide; it provides a solid foundation for patients navigating a complex condition 😊
josh Furley
July 11, 2023 AT 09:03Indeed, the synergistic integration of pulmonology and obstetrics protocols optimizes perinatal outcomes 🚀