
Diabetic retinopathy isn't just a complication of diabetes-it's the leading cause of preventable blindness in adults under 65. If you have diabetes, skipping your eye checkups isn't a time-saver-it’s a risk you can’t afford. The good news? With the right screening schedule and timely treatment, up to 98% of severe vision loss from this condition can be avoided. But knowing when to get checked and what treatments actually work isn’t as simple as ‘once a year.’ The rules have changed. And if you’re still getting screened annually regardless of your risk level, you might be doing more harm than good.
Who Needs Screening and When?
Not everyone with diabetes needs an eye exam every 12 months. That outdated rule is being replaced by smart, personalized schedules based on your actual risk. For people with type 2 diabetes, if you’ve had two clean screenings back-to-back and your HbA1c is under 7%, blood pressure is controlled, and you have no signs of kidney damage, you can safely extend your screening to every 2-3 years. Some low-risk patients may even go 4-5 years between exams, according to the UK National Screening Committee and recent studies.
But here’s the catch: if you have type 1 diabetes, you’re not eligible for that extension. Your first eye exam should happen 3-5 years after diagnosis, then follow the same risk-based schedule. And if you already have any level of retinopathy-even mild-you need to be seen more often. No exceptions.
Screening isn’t just a quick glance. It’s a detailed digital photo of the back of your eye, taken with a special camera after your pupils are dilated. Two images per eye, covering the central and outer retina. This isn’t something your primary care doctor can do with a flashlight. It requires trained technicians and certified image graders. In rural areas, where access is limited, telemedicine platforms are stepping in. A smartphone-based camera like the D-Eye device can capture images your eye doctor reviews remotely-9 out of 10 times, it catches what a specialist would see.
How Screening Intervals Are Decided
Screening schedules aren’t random. They’re calculated using real data. The RetinaRisk algorithm, validated in a 2023 study, looks at five key factors: how long you’ve had diabetes, your average blood sugar (HbA1c), your blood pressure, your kidney function (eGFR), and whether you already have retinopathy. Based on that, it tells your doctor whether you should be screened in 6 months, 12 months, or 5 years.
For example:
- No retinopathy + HbA1c < 7% + BP < 140/90 + normal kidney function → Screen every 3-4 years
- Mild nonproliferative retinopathy → Come back in 12 months
- Moderate nonproliferative retinopathy → See an eye specialist within 3-6 months
- Severe nonproliferative retinopathy → Must be evaluated within 3 months
- Proliferative retinopathy or diabetic macular edema → See an eye doctor within 1 month
That last one is critical. Proliferative retinopathy means new, fragile blood vessels are growing in your eye. They leak. They bleed. They scar. And they can pull your retina off. Waiting six months could mean losing your vision for good.
What Happens If Retinopathy Is Found?
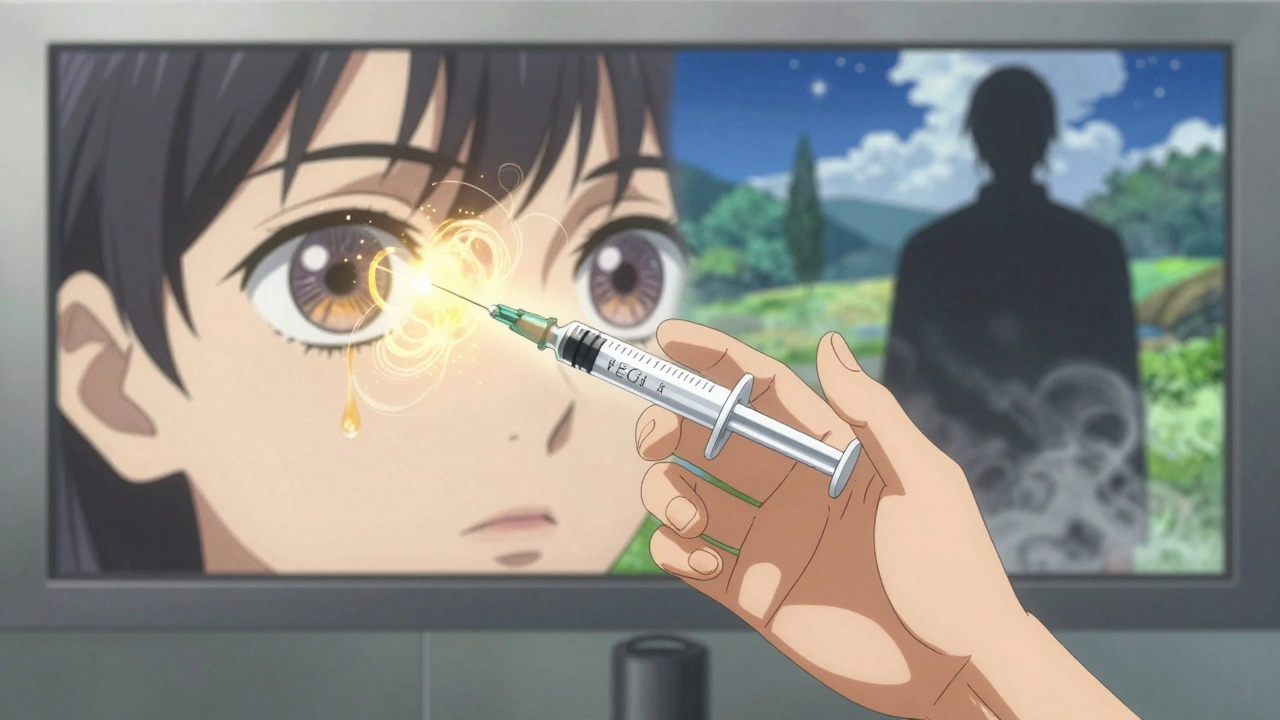
Not every case needs treatment right away. Mild cases are monitored. But if your doctor sees signs of sight-threatening damage, you’ll be referred to a retinal specialist. The two main treatments today are laser therapy and injections.
Laser treatment (panretinal photocoagulation) is used for proliferative retinopathy. It doesn’t restore vision-it stops it from getting worse. The laser creates tiny burns on the outer retina, which reduces the demand for oxygen and causes abnormal blood vessels to shrink. It’s not fun. It can cause night vision loss or blind spots. But it cuts the risk of severe vision loss by more than 50%.
For diabetic macular edema-the swelling in the center of your retina-anti-VEGF injections are the gold standard. Drugs like aflibercept, ranibizumab, and bevacizumab are injected directly into your eye. They block the protein that causes leaking blood vessels. Most patients need 3-6 injections in the first year, then maintenance shots every 2-4 months. Studies show these injections can improve vision in up to 40% of patients and stabilize it in another 40%.
There’s also a newer option: corticosteroid implants. These tiny devices are placed inside the eye and slowly release medicine over several months. They’re used when anti-VEGF drugs don’t work well enough. But they come with risks-higher chance of cataracts and elevated eye pressure.
Why Your Blood Sugar and Blood Pressure Matter More Than You Think
Treatment isn’t just about eye shots and lasers. The real game-changer is what you do outside the clinic. The DCCT and EDIC studies proved it: keeping your HbA1c below 7% cuts your risk of developing retinopathy by 76% if you have type 1 diabetes. For type 2, it slows progression by over half. That’s not a suggestion-it’s medical fact.
Blood pressure matters too. If your systolic pressure is above 140 mmHg, your risk of retinopathy jumps. Keeping it under 130/80 helps protect your eyes as much as your kidneys and heart. And if your kidneys are starting to fail (eGFR below 60), your eyes are in danger too. That’s why your doctor checks your urine for protein and your blood for creatinine every year.
Even short-term spikes in blood sugar can damage blood vessels. If your HbA1c swings wildly-say, from 6.5% to 9% and back-your eyes are under constant stress. Stability matters more than perfection.
What About AI and New Tech?
Artificial intelligence is changing screening fast. Google’s DeepMind algorithm, tested on over 11,000 retinal images, matched or beat human graders in detecting sight-threatening retinopathy. The FDA cleared the first AI system for autonomous screening in 2018-IDx-DR. Now, some clinics use AI to read your photos before a doctor even looks. It flags the high-risk cases and lets the specialist focus on what needs urgent attention.
These tools are especially helpful in places with few eye doctors. In rural counties where 1 in 5 people can’t get to an ophthalmologist, tele-screening with AI is saving sight. The technology isn’t perfect-it can miss subtle swelling or misread cataracts-but when combined with human review, it’s incredibly accurate.
Future tools are even simpler. Devices like the D-Eye adapter turn your smartphone into a retinal camera. Primary care nurses can take pictures during routine visits. Results are sent to a specialist within hours. This isn’t science fiction-it’s happening now in community clinics across the U.S. and the UK.
What Patients Are Saying
On Reddit, people with diabetes are split. One user, Type1Warrior87, says switching from yearly to biennial screenings reduced his anxiety: “I finally feel like my care is tailored to me, not just a checkbox.” Another, RetinaScared2023, wasn’t so lucky: “They pushed for 2-year intervals even though my HbA1c was 8.5%. I got macular edema. I wish I’d stuck with annual exams.”
That’s the problem. Risk-stratified screening only works if your doctor knows your numbers and applies the guidelines correctly. If your clinic doesn’t track HbA1c trends or ignores your blood pressure, you’re stuck on the old schedule. Don’t assume your doctor is using the latest protocol. Ask: “Based on my HbA1c, BP, and kidney results, what’s my retinopathy risk level?” If they can’t answer, it’s time to push for better.
Survey data from the NHS shows 87% of patients are happy with risk-based screening. They save time, money, and stress. But 13% worry they’ll miss something. That’s why clear communication matters. You should leave every appointment knowing your risk level, your next due date, and what warning signs to watch for-blurred vision, floaters, dark spots.
What’s Next for Diabetic Eye Care
The global market for diabetic retinopathy screening is exploding-projected to hit $4.7 billion by 2028. Why? Because diabetes is rising fast. By 2045, nearly 700 million people will have it. And without better screening, millions will lose their sight.
The World Health Organization estimates that scaling up risk-based screening could prevent 2.5 million cases of blindness by 2030. But only if we fix the gaps. Right now, low-income communities see 2.3 times more vision loss from diabetes than wealthier ones-even though their diabetes rates are similar. Access to screening, consistent follow-up, and affordable treatments aren’t equally available.
The future isn’t just about better cameras or smarter AI. It’s about making sure everyone, no matter where they live or how much they earn, gets the same chance to keep their vision.
Key Takeaways
- Annual screening isn’t always needed-risk-based intervals are now standard.
- Low-risk type 2 diabetes patients can safely wait 2-4 years between eye exams.
- Anyone with any level of retinopathy needs more frequent monitoring.
- Anti-VEGF injections and laser therapy are the two main treatments for sight-threatening damage.
- Your HbA1c and blood pressure are the biggest factors in preventing progression.
- AI and smartphone-based screening are making eye care more accessible than ever.
- If your clinic doesn’t use your HbA1c, BP, or kidney results to set your schedule, ask why.



Webster Bull
December 14, 2025 AT 05:19Man, I used to skip my eye checks like they were optional yoga classes. Then I got the scare of my life-floaters, blurry vision, the whole nightmare. Turns out my HbA1c was creeping up and my doc didn’t even check my kidney numbers. Now I know: it’s not about being perfect, it’s about being consistent. Small wins save sight.
Scott Butler
December 15, 2025 AT 05:47This whole risk-based screening is just another liberal scam to cut costs. Back in my day, we got checked every year like clockwork. No algorithms, no excuses. If you’re diabetic, you get your eyes looked at-period. The government’s trying to replace doctors with spreadsheets and it’s dangerous.
Ronan Lansbury
December 15, 2025 AT 14:11Of course they’re pushing ‘personalized’ screening. The pharmaceutical-industrial complex needs you to think you’re safe so you stop asking questions. AI? Please. Those algorithms are trained on data from people who can afford insulin, not the folks in rural Alabama. This isn’t medicine-it’s market segmentation dressed in white coats.
And don’t get me started on ‘smartphone cameras.’ You think a $50 adapter can replace a retinal specialist? Wake up. This is how they privatize healthcare until only the rich can see clearly.
sharon soila
December 16, 2025 AT 17:01I want to thank you for writing this with such care. I’m a type 2 diabetic and I didn’t realize my blood pressure was hurting my eyes too. I thought only sugar mattered. Now I track everything-HbA1c, BP, even my urine test results. I feel empowered, not scared. You gave me the tools to take back my health. Thank you.
nina nakamura
December 18, 2025 AT 05:49People who skip annual screenings are idiots. You think your HbA1c is ‘under 7’? Prove it. Did you get your A1c tested last month or just guess? Most people lie to themselves. I’ve seen too many lose vision because they trusted a ‘risk calculator’ instead of their doctor. Annual. Every. Single. Year. No excuses.
Tom Zerkoff
December 19, 2025 AT 02:15This is one of the clearest, most compassionate summaries of diabetic eye care I’ve ever read. Thank you for highlighting that stability matters more than perfection. Many patients feel guilty when their numbers aren’t perfect-but the real enemy is inconsistency, not occasional spikes. The fact that AI and telemedicine are reaching rural communities? That’s hope in action. Let’s make sure no one gets left behind.
Sheldon Bird
December 20, 2025 AT 20:24Just had my first AI-screened eye check last week. Took 5 minutes. Nurse took pics with my phone. Doctor reviewed it the same day. No dilation, no waiting. I cried. Not because I was scared-because I finally felt seen. 🙏
Karen Mccullouch
December 22, 2025 AT 15:43Ugh I’m so tired of people acting like this is some breakthrough. My cousin lost his vision because he trusted this ‘risk-based’ nonsense. His HbA1c was 8.2 and they told him to wait two years. He woke up blind. Now he’s on disability. Don’t let them gaslight you. If you’re diabetic, your eyes are ticking time bombs. Get checked every year. Period. End of story.
Michael Gardner
December 22, 2025 AT 17:56Wait, so if I have type 1 diabetes but my HbA1c is 6.8, BP is 125/75, and my kidneys are perfect… I still can’t go 2 years? But if I had type 2 with the same numbers I could? That’s not risk-based-that’s discrimination by diagnosis. Who decided type 1 is inherently worse? Is that even medically sound or just old-school bias?