CYP450 Drug Interaction Checker
Check Medication Interactions
This tool shows if two medications compete for the same CYP450 enzyme metabolism pathway.
Interaction Result
Important Safety Information
CYP450 enzymes process 90% of medications. If two drugs compete for the same enzyme, levels of one or both drugs can increase dangerously or decrease to ineffective levels.
Always tell your doctor and pharmacist about all medications including supplements. Never take new drugs without checking interactions. Report symptoms like fatigue, muscle pain, dizziness, or irregular heartbeat immediately.
Timing medications doesn't help. CYP450 interactions happen at the enzyme level, not timing. The only safe approach is avoiding combinations or switching to different pathways.
Imagine taking your morning pill for high blood pressure, then adding a common antibiotic for a sinus infection - and not realizing you just doubled the risk of a dangerous heart rhythm. This isn’t science fiction. It’s happening every day because of something called CYP450 enzyme interactions.
What Are CYP450 Enzymes and Why Do They Matter?
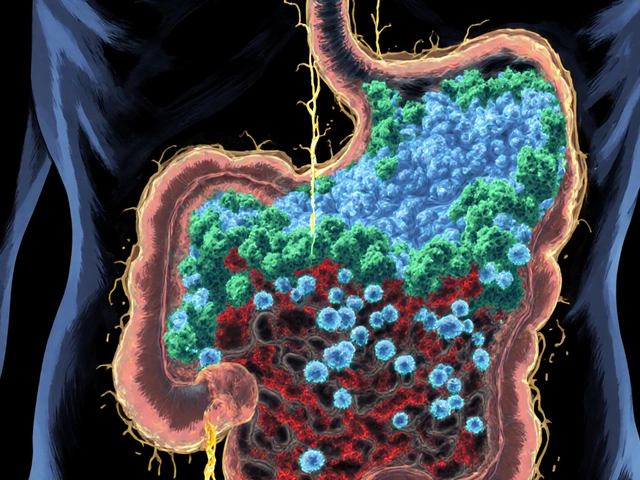
Your body doesn’t just absorb drugs and call it a day. It has to break them down - and that’s where CYP450 enzymes come in. These are proteins, mostly in your liver, that act like molecular scissors. They chop up drugs so your body can flush them out. About 90% of all prescription medications rely on these enzymes to be processed. That includes statins, antidepressants, painkillers, blood thinners, and even some cancer drugs. There are six main CYP450 enzymes that handle most of this work. CYP3A4 is the biggest player, dealing with half of all drugs. CYP2D6 handles a quarter, including many antidepressants and beta-blockers. CYP2C9, CYP2C19, CYP1A2, and CYP2E1 split the rest. Together, these six enzymes manage 90% of drug metabolism. The other 10% go through different pathways, like kidney excretion or glucuronidation. But if your drug relies on CYP450, you’re in the middle of a high-stakes competition.The Competition: How Drugs Fight for Space
Think of CYP450 enzymes as busy toll booths. Each drug needs to pass through one to get metabolized. When two drugs need the same enzyme, they fight for space. The stronger one wins - and the loser gets stuck. This fight happens in two ways: inhibition and induction. Inhibition is like someone cutting in line. One drug blocks the enzyme’s active site, so the other can’t get through. This is the most common cause of dangerous interactions. For example, clarithromycin (an antibiotic) strongly inhibits CYP3A4. If you’re taking simvastatin (a cholesterol drug) that also uses CYP3A4, adding clarithromycin can cause simvastatin levels to spike 10-fold. That’s how a simple infection treatment led to rhabdomyolysis - muscle breakdown - in a 72-year-old woman. Her kidneys couldn’t handle the overload. Some inhibitors are so strong they permanently damage the enzyme. It takes days for your body to make new ones. That’s why the effects linger even after you stop the interfering drug. Induction is the opposite. Some drugs, like rifampin (used for tuberculosis) or St. John’s wort (a popular herbal supplement), tell your liver to make more CYP450 enzymes. Suddenly, your body becomes a drug-processing machine on overdrive. If you’re on birth control or an antirejection drug, this can drop its levels so low that it stops working. A transplant patient on cyclosporine who starts taking St. John’s wort might reject their new organ - all because the enzyme got too efficient.Genetics: Why Your Body Handles Drugs Differently
Not everyone processes drugs the same way. Your genes decide whether you’re a slow, normal, or super-fast metabolizer. This is especially true for CYP2D6. About 5-10% of Caucasians are poor metabolizers - their bodies barely break down drugs like codeine or metoprolol. For them, a standard dose can cause toxicity. On the other end, ultrarapid metabolizers (1-10% of people, depending on ancestry) break down drugs so fast they don’t work at all. A mother giving codeine to her child for pain? If she’s an ultrarapid metabolizer, her breast milk could contain dangerous levels of morphine. CYP2C19 is another big one. About 30% of Caucasians and 60% of Asians are intermediate metabolizers for this enzyme. That means clopidogrel, a blood thinner often given after a heart attack, won’t work properly for them. The FDA now recommends genetic testing before prescribing it. Without it, you’re just taking a pill that does nothing.
Real-World Examples You Should Know
Here are some common, dangerous combinations that show up in clinics every week:- SSRIs + beta-blockers: Fluoxetine and paroxetine inhibit CYP2D6. If you’re on metoprolol for high blood pressure, adding one of these SSRIs can slow down metoprolol’s breakdown. Result? Your heart rate drops dangerously low. Nurses report this happens in 15-20% of patients.
- Theophylline + fluvoxamine: Fluvoxamine is a strong CYP1A2 inhibitor. Theophylline (used for asthma) is metabolized by CYP1A2. One patient’s theophylline level jumped from 10 to 25 mcg/mL in 48 hours - enough to trigger seizures.
- Grapefruit juice + statins: Grapefruit doesn’t just taste bitter - it blocks intestinal CYP3A4. That means more of your statin gets absorbed. One glass can reduce clearance by 30-80%. For some statins, that’s enough to cause muscle damage.
- Warfarin + CYP2C9 inhibitors: Warfarin has a narrow safety window. Even a small increase in its levels can cause bleeding. Drugs like amiodarone or fluconazole can push it over the edge.
How to Stay Safe
You don’t need to be a pharmacist to avoid these traps. Here’s what works:- Always tell your doctor and pharmacist every medication you take - including vitamins, herbs, and over-the-counter pills. St. John’s wort, garlic supplements, and even cranberry juice can interfere.
- Ask: “Is this drug processed by CYP3A4, CYP2D6, or CYP2C9?” If you’re on two drugs that use the same enzyme, ask if they’re safe together.
- Use trusted interaction checkers. Tools like Lexicomp are used in hospitals because they catch 95% of major interactions. If your pharmacy uses one, ask them to run a check before you leave with a new prescription.
- Don’t ignore side effects. Unexplained fatigue, muscle pain, dizziness, or irregular heartbeat after starting a new drug? It could be an interaction.
- Consider genetic testing. If you’re on multiple long-term meds - especially antidepressants, blood thinners, or painkillers - a simple saliva test can tell you if you’re a poor or ultrarapid metabolizer. Tests cost $250-$500 and take about a week. For people on five or more drugs, it’s worth it.
What’s Changing in 2025
The field is moving fast. By 2024, 75% of major electronic health records (like Epic and Cerner) now warn doctors in real time when a dangerous interaction is about to happen. That’s a big win. But adoption is uneven. Only 28% of primary care doctors routinely check for CYP450 interactions, compared to 42% of pharmacists. The FDA now requires all new drugs to include detailed CYP450 interaction info on their labels. And by 2025, the NIH plans to standardize how we name CYP450 gene variants worldwide - making testing more accurate and consistent. AI tools like IBM Watson for Drug Interactions are entering beta testing. They can predict CYP450 interactions with 89% accuracy. In the next few years, your doctor might get an alert that says: “Patient has CYP2D6 poor metabolizer status. Avoid codeine. Use tramadol instead.”The Bigger Picture
CYP450 interactions are the #1 modifiable cause of bad drug reactions in people taking five or more medications. They cause 15-20% of hospitalizations in older adults. And yet, most people have never heard of them. The good news? You don’t need to memorize enzyme names. You just need to be aware that drugs don’t work in isolation. Your body is a busy system. What you take today can change how everything else works tomorrow. If you’re on multiple medications - especially if you’re over 65, have heart disease, or take antidepressants - ask your pharmacist to run a drug interaction check. It takes five minutes. It could save your life.What drugs are most likely to cause CYP450 interactions?
The biggest culprits are strong inhibitors or inducers. Strong inhibitors include clarithromycin, ketoconazole, fluoxetine, paroxetine, fluvoxamine, and grapefruit juice. Strong inducers include rifampin, carbamazepine, phenytoin, and St. John’s wort. These can change the levels of other drugs by 50-90%. Always check if a new medication is on this list before taking it.
Can I avoid CYP450 interactions by taking my meds at different times?
No. Timing doesn’t help. CYP450 inhibition or induction happens at the enzyme level - not the timing level. If two drugs compete for the same enzyme, taking them 12 hours apart won’t make a difference. The enzyme is still blocked or overworked. The only safe approach is avoiding the combination entirely or switching to a drug that uses a different metabolic pathway.
Are herbal supplements safe if they’re natural?
No. Many herbal products are potent CYP450 modulators. St. John’s wort induces CYP3A4 and CYP2C9, making birth control, antidepressants, and transplant drugs fail. Garlic and ginkgo inhibit CYP2C9 and CYP3A4, increasing bleeding risk with warfarin. Green tea can inhibit CYP3A4. Just because something is natural doesn’t mean it’s safe - especially with prescription meds.
What should I do if I think I’m having a CYP450 interaction?
Stop the new medication immediately and contact your doctor or pharmacist. Symptoms like unexplained fatigue, muscle pain, dizziness, irregular heartbeat, confusion, or bleeding are red flags. Don’t wait. Bring a list of all your medications - including supplements - to your appointment. If you’re on warfarin, statins, or antidepressants, these interactions can be life-threatening.
Is genetic testing for CYP450 worth it?
Yes, if you’re on three or more long-term medications, especially for mental health, heart disease, or chronic pain. Testing can tell you if you’re a poor or ultrarapid metabolizer for key enzymes like CYP2D6, CYP2C19, or CYP2C9. This helps avoid ineffective treatment or dangerous side effects. Many insurance plans cover it now, especially if you’ve had a bad reaction before. It’s not a one-time fix - it’s lifelong guidance for your prescriptions.



Dave Alponvyr
December 17, 2025 AT 00:18So basically, grapefruit juice is the ultimate drug saboteur. One glass and your statin turns into a wrecking ball. Thanks, nature.
Ron Williams
December 18, 2025 AT 03:50I’ve seen this play out in my grandma’s meds. She was on warfarin, then started taking that ‘natural’ heart supplement. Ended up in the ER with a bruise the size of a dinner plate. Never ask a friend for supplement advice - ask a pharmacist.
Aditya Kumar
December 19, 2025 AT 10:18Too much info. I just take my pills and hope for the best.
Billy Poling
December 19, 2025 AT 15:31It is of paramount importance to underscore that the cytochrome P450 system, a highly conserved enzymatic cascade primarily localized within the endoplasmic reticulum of hepatocytes, serves as the principal metabolic pathway for the biotransformation of xenobiotics, including but not limited to pharmaceutical agents, dietary constituents, and phytochemicals. The competitive inhibition or transcriptional upregulation of isoforms such as CYP3A4, CYP2D6, and CYP2C9 may result in clinically significant pharmacokinetic alterations, leading to either toxic accumulation or subtherapeutic concentrations of concomitantly administered medications. Therefore, it is imperative that clinicians and patients alike engage in comprehensive medication reconciliation and consult authoritative drug interaction databases prior to polypharmacy initiation.
Randolph Rickman
December 20, 2025 AT 05:09This is why I always tell my patients: your meds aren’t just floating around in a vacuum. They’re in a crowded elevator with no exit. If you’re on five drugs, you’re basically playing Russian roulette with your liver. But here’s the good news - you can win. Ask your pharmacist for a med review. It’s free. It takes five minutes. And it might keep you out of the hospital. Seriously, do it. Your future self will thank you.
Tiffany Machelski
December 20, 2025 AT 12:14i had no idea grapefruit could do that… i drink it every mornin. oops. also, is st. johns wort the same as the one in the little bottle at walmart? lol
Souhardya Paul
December 22, 2025 AT 09:44Love how this breaks it down without jargon. I’m a nurse and I still get tripped up by CYP2C19 and clopidogrel. My favorite tip? If you’re on more than three meds, print out your list and take it to your pharmacist. They’ll catch things your doctor misses. And yeah - genetic testing? Totally worth it if you’ve had weird side effects before. Mine said I’m a slow CYP2D6 metabolizer - explains why codeine never worked and tramadol made me feel like a robot.
Josias Ariel Mahlangu
December 23, 2025 AT 17:53People think natural means safe. That’s the problem. You don’t see the warning labels on herbs. You don’t see the FDA logo. But your liver doesn’t care. It just sees poison. You think you’re being healthy - you’re just poisoning yourself slowly. Shame.