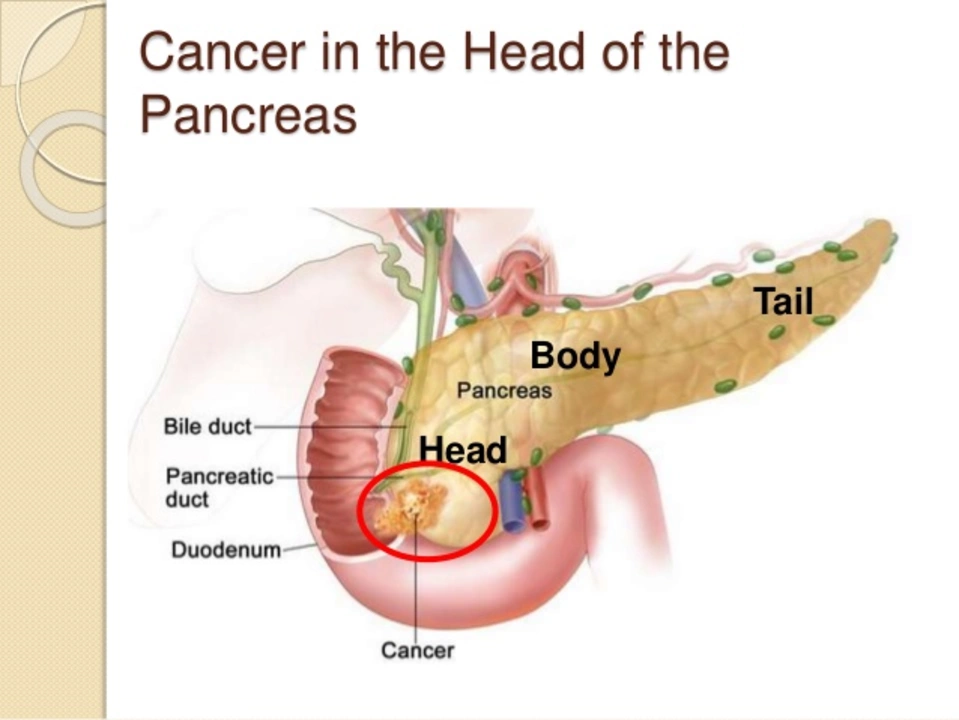
Introduction: Understanding Pancreatic Cancer
Pancreatic cancer is a type of cancer that starts in the pancreas, a vital organ located behind the stomach and responsible for producing hormones and enzymes required for digestion. Unfortunately, pancreatic cancer is often challenging to detect and diagnose early, resulting in a low survival rate. In this article, we will explore the symptoms, causes, and risk factors of pancreatic cancer, helping you gain a better understanding of this deadly disease and what to look out for.
Common Symptoms of Pancreatic Cancer
One of the reasons pancreatic cancer is difficult to diagnose is because its symptoms may be vague or mimic other conditions. However, there are some common signs and symptoms to watch out for, including:
- Jaundice (yellowing of the skin and eyes)
- Abdominal or back pain
- Unexplained weight loss
- Loss of appetite
- Nausea and vomiting
- Changes in stool color and consistency
- New-onset diabetes
- Fatigue and weakness
It's essential to pay attention to these symptoms and consult with a healthcare professional if you experience any of them, especially if they persist or worsen.
Potential Causes of Pancreatic Cancer
While the exact cause of pancreatic cancer is still not fully understood, researchers believe that genetic mutations in the DNA of pancreatic cells lead to the development of cancer. These mutations cause the cells to grow uncontrollably and form a tumor. Some factors may increase the risk of these genetic mutations occurring, such as exposure to certain chemicals or a family history of pancreatic cancer.
Genetic Factors and Family History
Approximately 5-10% of pancreatic cancer cases are believed to be hereditary, meaning they result from gene mutations passed down from one generation to another. Having a close relative (parent, sibling, or child) with pancreatic cancer increases your risk of developing the disease. Additionally, certain inherited gene mutations, such as those associated with BRCA2, Lynch syndrome, or familial atypical multiple mole melanoma (FAMMM) syndrome, can also increase the risk of pancreatic cancer.
Age, Gender, and Race as Risk Factors
Age plays a significant role in the risk of developing pancreatic cancer, as the majority of cases are diagnosed in people over 45 years old, with the average age at diagnosis being 70. Men are slightly more likely to develop pancreatic cancer than women, and African Americans have a higher risk than people of other races. However, the reasons for these disparities are not well understood and may be related to genetic, environmental, or lifestyle factors.
Smoking and Alcohol Consumption
Smoking is a significant risk factor for pancreatic cancer, with smokers being two times more likely to develop the disease than non-smokers. Quitting smoking can significantly reduce this risk, making it an essential preventive measure. Additionally, heavy alcohol consumption has been linked to pancreatic cancer, especially when combined with smoking. Limiting alcohol intake and avoiding smoking can help lower your risk of developing this deadly disease.
Obesity and Poor Diet
Obesity is another risk factor for pancreatic cancer, with people who are obese having a 20% higher risk of developing the disease compared to those with a healthy weight. A diet high in red and processed meats has also been linked to an increased risk of pancreatic cancer, while consuming fruits, vegetables, and whole grains can help reduce this risk. Maintaining a healthy weight and eating a balanced diet can play a crucial role in preventing pancreatic cancer.
Chronic Pancreatitis and Diabetes
Chronic pancreatitis, a long-term inflammation of the pancreas, can increase the risk of pancreatic cancer. Some factors that can cause chronic pancreatitis, such as heavy alcohol consumption and smoking, are also risk factors for pancreatic cancer. Additionally, people with diabetes, especially type 2 diabetes, have a higher risk of developing pancreatic cancer. However, more research is needed to understand the relationship between diabetes and pancreatic cancer fully.
Final Thoughts: Prevention and Early Detection
While pancreatic cancer is a challenging disease to diagnose and treat, understanding its symptoms, causes, and risk factors can help you take steps to reduce your risk and be vigilant about early detection. Maintain a healthy lifestyle, pay attention to any potential symptoms, and consult with a healthcare professional if you have concerns about your risk of developing pancreatic cancer. Early detection and intervention can significantly improve the chances of successful treatment and survival.



Brennan Keeler
May 28, 2023 AT 01:05Listen up, folks-if you keep chowing down on processed meats and ignore basic hygiene, you’re practically signing a death warrant for your pancreas. The state of your diet is a moral issue, and we must hold each other accountable. No more excuses, stop the junk and start a regezimen that respects your body’s engineering.
Chelsea Hackbarth
June 6, 2023 AT 11:05🙌 Absolutely spot‑on! The link between smoking and pancreatic risk is crystal clear, and swapping that habit for a brisk walk can make a massive difference. Keep spreading the knowledge! 😊
Adam Shooter
June 15, 2023 AT 21:05The epidemiological data delineates a multifactorial etiopathogenesis wherein synergistic carcinogenic vectors-namely, tobacco‑derived nitrosamines, ethanol metabolites, and adiposity‑linked insulin resistance-coalesce to potentiate oncogenic transformation within the exocrine pancreas. From a mechanistic standpoint, chronic inflammation precipitates somatic DNA damage via reactive oxygen species, thereby engendering mutational hotspots in KRAS and TP53 loci. Moreover, the demographic stratification elucidated in the literature underscores a disproportionate incidence among cohorts with elevated BMI, which ostensibly modulates the tumor microenvironment through adipokine dysregulation. Hence, the intersectionality of lifestyle, genetics, and environmental exposure constructs a complex risk matrix that warrants granular scrutiny.
Shanmughasundhar Sengeni
June 25, 2023 AT 07:05Yo, that was a mouthful. In plain English: smoking, booze, and being overweight are the big bad guys for your pancreas. If you’re not already on board with quitting, start now. Nobody’s got time for regret.
ankush kumar
July 4, 2023 AT 17:05Pancreatic cancer remains one of the stealthiest malignancies, often slipping past early detection thresholds. Its insidious nature is compounded by nonspecific symptoms that mimic benign gastrointestinal disorders. Consequently, many patients receive a diagnosis only after the disease has progressed to an advanced stage. Lifestyle modification stands as a cornerstone of primary prevention, yet adherence rates are disappointingly low in many populations. Regular aerobic exercise not only improves insulin sensitivity but also attenuates systemic inflammation, both of which are protective against neoplastic transformation. Dietary patterns rich in antioxidants, fiber, and phytonutrients have been shown to modulate carcinogenic pathways at the cellular level. Conversely, high consumption of red and processed meats introduces heterocyclic amines that can directly damage pancreatic DNA. Smoking introduces a plethora of carcinogenic compounds, including nitrosamines, which accumulate in pancreatic tissue and instigate mutagenesis. Alcohol, especially when consumed in binge episodes, precipitates chronic pancreatitis, creating a fertile ground for malignant change. Genetic predisposition, such as BRCA2 and PALB2 mutations, magnifies the impact of these environmental insults, lowering the threshold for tumor initiation. Early screening protocols, like endoscopic ultrasound for high‑risk families, have demonstrated improved survival outcomes when lesions are resected promptly. However, access to such specialized diagnostics is uneven, often limited by socioeconomic barriers. Patient education initiatives must therefore emphasize symptom awareness, encouraging prompt medical evaluation for unexplained weight loss or jaundice. Health policies should allocate resources toward community‑based programs that facilitate smoking cessation and nutrition counseling. Ultimately, a concerted effort integrating lifestyle, genetics, and healthcare infrastructure offers the best hope for reducing the devastating burden of pancreatic cancer.
Cameron White
July 14, 2023 AT 03:05Ever notice how every major pharma story hides a hidden agenda? The push for early detection tests seems more like a cash‑cow scheme than a genuine health initiative. Stay vigilant.
Amélie Robillard
July 23, 2023 AT 13:05😏 Oh sure, because the only thing more trustworthy than a multi‑billion‑dollar pharma lobby is a random blog post. Let’s just trust the “experts” who never admit they’re motivated by profit. 🙃
Fae Wings
August 1, 2023 AT 23:05It’s heartbreaking to think how many families are torn apart because we ignore these warning signs. The silent ache of lost time, the lingering hope that maybe-just maybe-something could have been caught earlier.
Anupama Pasricha
August 11, 2023 AT 09:05From a public health perspective, integrating pancreatic risk assessment into routine check‑ups could bridge the current detection gap. Utilizing non‑invasive biomarkers alongside patient history may flag high‑risk individuals earlier.
Bryce Charette
August 20, 2023 AT 19:05Great point! Just make sure the terminology stays consistent-use “risk assessment” throughout and avoid swapping in “screening” unless you’re talking about a specific test. Small edits can keep the article sharp.
Christina Burkhardt
August 30, 2023 AT 05:05Adding a quick reference table summarizing risk factors-age, smoking, obesity, family history-would give readers a handy visual. It’s a minor addition, but it can significantly improve comprehension.
liam martin
September 8, 2023 AT 15:05In the end, knowledge is the only weapon we truly have.