When a patient takes a pill that combines two drugs - say, a blood pressure medicine and a diuretic - they expect it to work just like the brand-name version. But getting a generic version of that combo to perform the same way isn’t as simple as copying a single-drug tablet. Bioequivalence for combination products is one of the toughest puzzles in generic drug development today. It’s not just about matching how much drug gets into the bloodstream. It’s about proving that every active ingredient in the mix behaves the same way, under real-world conditions, every single time. And that’s where things get messy.
Why Combination Products Are So Hard to Copy
Most generic drugs are single-ingredient pills. The rules for those are well-established: compare the rate and amount of drug absorbed in healthy volunteers. If the generic’s peak concentration (Cmax) and total exposure (AUC) fall within 80-125% of the brand, it’s approved. Simple. But combination products? They break that model. Fixed-dose combinations (FDCs) - like those for HIV, diabetes, or hypertension - combine two or more active ingredients in one tablet. The problem? Those ingredients can interact. One might slow down the absorption of the other. Or change how it’s metabolized. A 2022 FDA report found that 73% of new drugs approved between 2010 and 2019 were complex products like these. And yet, the testing rules haven’t kept pace. The FDA now requires generic makers to prove bioequivalence not just to the combo product itself, but also to each individual drug given separately. That means running three-way crossover studies: one group gets the generic combo, another gets the brand combo, and a third gets the two drugs taken apart. That’s expensive. It’s time-consuming. And it often fails.The Topical Trap: Creams, Ointments, and Foams
If FDCs are tricky, topical products are worse. Think corticosteroid creams, antifungal ointments, or that foam for psoriasis. These aren’t swallowed. They’re applied to the skin. So how do you prove the drug gets where it needs to go? The FDA says use tape-stripping. Peel off 15-20 thin layers of the outer skin (stratum corneum) and measure how much drug is in each. Sounds precise? It’s not. There’s no standard on how thick each strip should be, how much pressure to use, or even how to analyze the samples. One lab’s results can vary 30% from another’s just because of technique. A 2024 study in Frontiers in Pharmacology showed that even with perfect lab conditions, tape-stripping only predicts actual skin absorption about 70% of the time. That’s why so many generic topical products get stuck in review. Mylan (now Viatris) spent over two years trying to launch a generic version of a calcipotriene/betamethasone foam. Three bioequivalence studies failed - not because the formula was wrong, but because the measurements didn’t match up consistently.Drug-Device Combos: The Inhaler Problem
Inhalers, auto-injectors, and nasal sprays are another nightmare. It’s not enough to prove the drug is the same. You have to prove the device delivers it the same way. For metered-dose inhalers, the particle size matters. Too big, and the drug hits the throat instead of the lungs. Too small, and it gets exhaled. The FDA requires aerosol particle size to be within 80-120% of the brand product. But getting that right? It takes specialized labs, calibrated equipment, and trained technicians. Even a tiny change in the valve or propellant can throw off the entire delivery. Dr. William Doub from the FDA said in 2024 that 65% of complete response letters for generic inhalers cite problems with the device. That’s not about chemistry. It’s about engineering. And most generic companies don’t have the expertise - or the budget - to tackle it.
Why So Many Studies Fail
The numbers don’t lie. A 2023 FDA report found that 35-40% of initial applications for modified-release FDCs fail bioequivalence testing. For topical products, failure rates are even higher. Why?- **Multiple analytes**: Two drugs mean two sets of data to track. One might pass, the other fails.
- **Formulation interactions**: One drug might bind to the other, changing how it dissolves.
- **Lack of standardized methods**: No one agrees on how to test skin absorption, inhalation, or even oral dissolution for complex combos.
- **Small sample sizes**: Studies often use 40-60 volunteers, but variability in absorption can mask true differences.
What’s Being Done - And What’s Still Missing
The FDA knows this is broken. In 2018, they launched the Complex Generic Products Initiative. Since then, they’ve issued 12 product-specific guidances. They’re working with NIST to create reference standards. They’re encouraging early meetings - Type II consultations - which have jumped 220% since 2020. One promising solution? Physiologically-based pharmacokinetic (PBPK) modeling. Instead of testing on people, companies use computer simulations to predict how the drug will behave in the body. The FDA has accepted PBPK models in 17 approved generic applications as of mid-2024. One case showed a 40% reduction in clinical testing needed. But here’s the catch: not every product can be modeled. And even when they can, regulators don’t always agree on the parameters. There’s still no universal standard.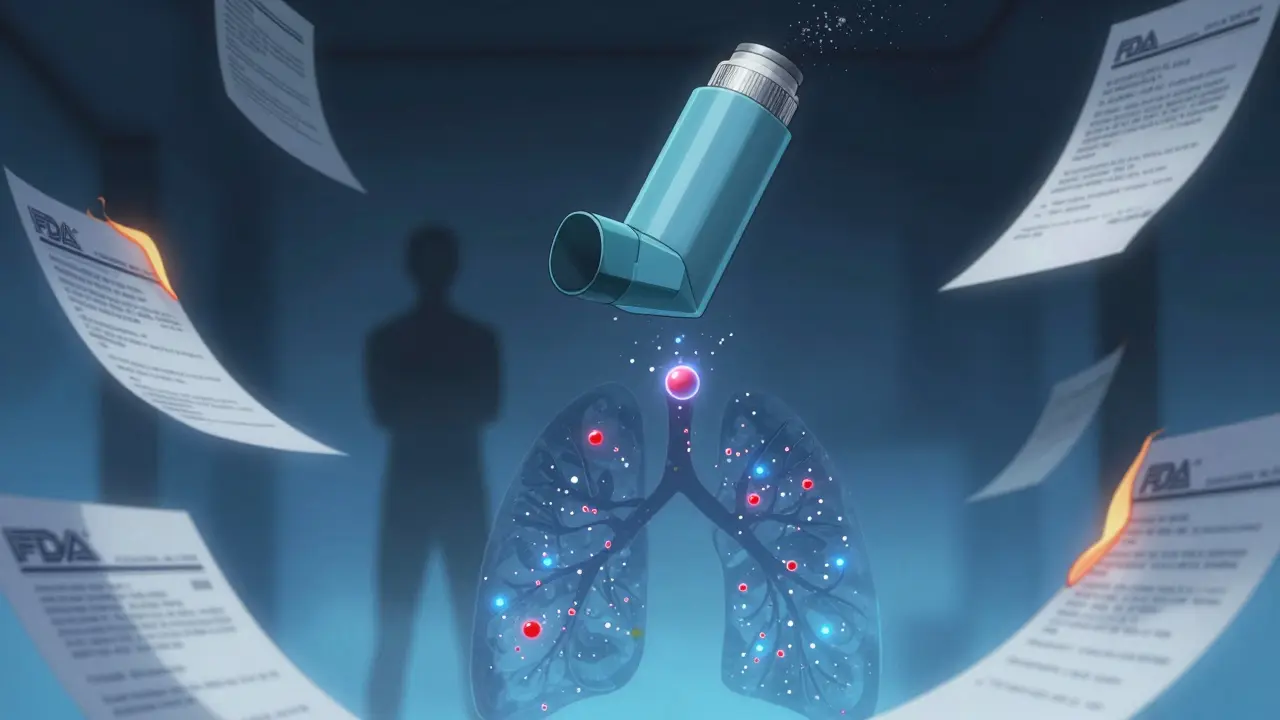
The Real Cost of Delay
Generic drugs saved the U.S. healthcare system $373 billion in 2020. But that savings doesn’t reach patients when the generics never get approved. As of June 2024, 312 combination products are on the FDA’s Complex Generic Drug Products list. Of those, 38% are topical, 22% are inhalers, and 19% are FDCs. The average approval time? 38.2 months - more than double the 14.5 months for simple generics. Meanwhile, patent thickets are growing. Between 2019 and 2023, lawsuits over combination products rose 300%. Each delay adds an average of 2.3 years before a generic can enter the market. The result? Patients pay more. Providers can’t switch. And innovation stalls.What Needs to Change
There’s no magic fix. But progress is possible:- **Standardize testing methods** - Especially for tape-stripping and inhaler performance. NIST’s reference standards are a start.
- **Expand PBPK modeling acceptance** - Make it mandatory for certain product types, with clear validation criteria.
- **Harmonize global rules** - EMA requires extra clinical data for 23% of submissions compared to FDA. That duplication adds 15-20% to development costs.
- **Create a fast-track pathway** - For products with proven safety profiles and no major interactions.
Final Thought: It’s Not About Cutting Corners
The goal isn’t to make generic approval easier. It’s to make it accurate. Patients deserve safe, affordable options. But cutting corners on bioequivalence doesn’t save money - it risks lives. The real challenge isn’t technical. It’s systemic. We need regulators, industry, and labs to work together - not in silos. We need data. We need standards. And most of all, we need to stop treating complex products like they’re just two pills in one.What is bioequivalence for combination products?
Bioequivalence for combination products means proving that a generic version delivers the same amount of each active ingredient into the body at the same rate as the brand-name product. For fixed-dose combinations, this includes proving equivalence to both the combo itself and to each individual drug taken separately.
Why are combination products harder to approve than single-drug generics?
Combination products involve multiple active ingredients that can interact, changing how each is absorbed or metabolized. Testing requires complex study designs, multiple analytical methods, and often, specialized equipment. Unlike single-drug generics, you can’t rely on a simple two-way crossover - you need three-way or even more complex protocols.
What’s the biggest hurdle for generic inhalers?
The biggest hurdle is the device, not the drug. Even tiny differences in valve design, propellant, or actuation force can change how the drug particles are delivered. The FDA requires aerosol particle size to be within 80-120% of the brand, and 65% of complete response letters cite device-related deficiencies.
How do topical products like creams fail bioequivalence testing?
Topical products fail because there’s no standard way to measure how much drug reaches the skin. Tape-stripping - the current method - varies widely between labs due to inconsistent technique. A 2024 study found only 70% predictability between lab results and actual skin absorption, leading to high failure rates.
Can computer modeling replace human trials for combination products?
Yes, in some cases. Physiologically-based pharmacokinetic (PBPK) modeling has been accepted in 17 approved generic applications as of mid-2024. It can reduce clinical testing by 30-50% by predicting how drugs behave in the body. But regulators still require real-world data for high-risk products, especially those with narrow therapeutic windows.
How long does it take to get a combination product approved as a generic?
On average, it takes 38.2 months for a complex combination product to get first-cycle approval from the FDA - more than double the 14.5 months for standard single-drug generics. Delays are often due to unclear testing methods, inconsistent feedback between FDA divisions, or failed bioequivalence studies.





Savannah Edwards
February 7, 2026 AT 02:43So I’ve been following this whole generic drug situation for years, mostly because my mom’s on a combo med for hypertension and diabetes, and we’ve had to switch brands twice in three years because the generics kept failing approval. It’s not just about cost-it’s about stability. You think you’ve got your routine down, then BAM, the new generic makes her dizzy or gives her weird nausea. And no one explains why. The FDA’s got these fancy guidances, but the real world? It’s chaos. Tape-stripping? Come on. How is a patient supposed to trust that a cream works if even the labs can’t agree on how to measure it? I’ve read studies where the same sample tested in two different labs gave 30% different results. That’s not science. That’s roulette with our health.
And don’t even get me started on inhalers. My cousin’s a respiratory therapist, and she says the aerosol particle size is everything. One tiny valve change, and instead of reaching the lungs, the drug just coats the throat. You’re not getting the dose. You’re just wasting money and breathing in propellant. We need better standards, not more paperwork. PBPK modeling? Yes, please. Let’s use computers to simulate what our bodies do, not drag 60 healthy volunteers through three-way crossover studies that cost $2 million each. That’s not innovation. That’s institutional inertia.
And yeah, I know some people say ‘but safety first!’-and I agree. But safety shouldn’t mean ‘never change.’ It should mean ‘change smartly.’ We’ve got the tech. We’ve got the data. We just need the will to stop treating combination products like they’re just two pills in a capsule. They’re not. They’re complex systems. And we’re treating them like they’re Legos.
Also, why does every single guidance document sound like it was written by a lawyer who hates humans? Can we please have plain language for once? I want to understand this, not file a FOIA request to decode it.